December 5, 2024
5 read me
This is a mutation to make the bird flu virus bind more effectively to human cells
A new study has found that tweaking a part of the H5N1 virus that infects dairy cows in one place could allow it to better attach to human cell receptors, raising concerns that it could spread more easily between people.
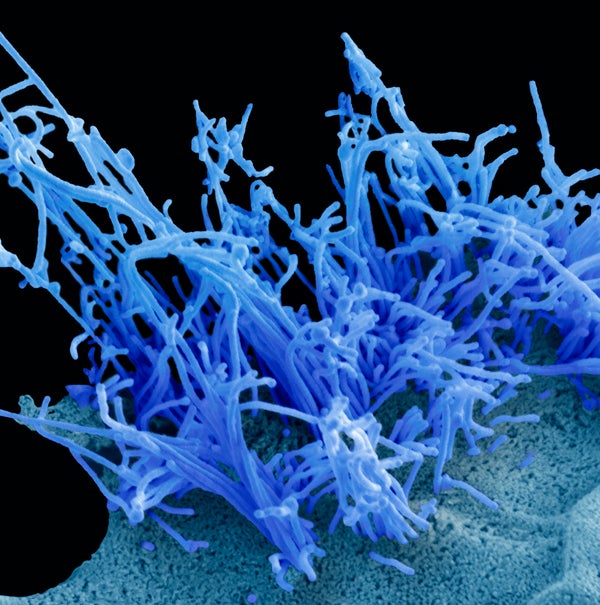
A human cell infected with the H5N1 avian influenza virus (blue filaments).
Steve Gschmeissner/Science Source
Scientists have found that H5N1, the highly pathogenic strain of avian influenza virus currently prevalent in US dairy cows, requires only a single mutation to readily adhere to human cells found in the upper respiratory tract. The findings were published today science, represent a potential one-step way to make the virus more efficient at human transmission, and it could have far-reaching consequences a new pandemic if such a mutation were to spread in nature.
Bird flu viruses are packed with surface proteins that allow them to bind to receptors on bird cells, allowing the virus to enter cells. The cell receptors in birds are different than in humans, but the variation is “very subtle,” says James Paulson, study author and a biochemist at Scripps Research. “For a new pandemic H5N1 virus, we know that the receptor specificity has to change from the bird type to the human type. So what will it take?” To his and his co-authors’ surprise, that switch required only one genetic change.
The particular group or clade of H5N1 responsible for the current outbreak was first detected in North America in 2021 and has caused large animal populationwild birds, bears, foxes, many marine mammals and, more recently, dairy cows. Since outbreaks of H5N1 in US dairy herds began this spring, human cases have mostly been linked to sick poultry or cattle, with most human infections. soft between farm workers at high risk of exposure (with some remarkable exceptions). There has been no evidence of human-to-human transmission, and the virus’s preference for receptor binding is a key obstacle to this.
About supporting science journalism
If you like this article, please consider supporting our award-winning journalism subscribe. By purchasing a subscription, you’re helping to ensure a future of impactful stories about the discoveries and ideas that shape our world.
“Obviously it’s speculative, but the better the virus binds to human receptors, it’s not great because it will probably lead to human-to-human transmission,” says Jenna Guthmiller, an immunologist at the University of Colorado Anschutz Medical Campus. , who was not involved in the new study.
The study authors focused on modifying one of H5N1’s surface proteins, hemagglutinin, which contains a binding site that allows the virus to attach to host cell receptors and initiate infection. The researchers created viral proteins from the genetic sequences of the isolated virus First human case in Texaswhich occurred in a person who developed bird flu after exposure to an infected cow. No live virus was used in the experiment. The scientists then engineered a series of different mutations into the amino acid chain, or protein building blocks, of hemagglutinin. A single mutation that swapped amino acid 226 in the sequence allowed H5N1 to switch its binding affinity from receptors on avian cells to receptors on human cells in the upper respiratory tract.
the past research Several flu mutations, including those tested in the new paper, are important in human receptor binding, Guthmiller says. These genetic adjustments have been marked in previous subtypes of influenza viruses that have caused human pandemics, such as those of 1918 and 2009. But viruses of the past usually needed at least two mutations to successfully change their preference for human receptors, explained co-author Ian Wilson. structural and computational biologist at Scripps. “This was amazing. (That) single mutation was enough to change receptor specificity,” he says.
Paulson added that the scientists who tested it in the new study had investigated the particular mutation in 2010 outbreaks of H5N1 in birds and some humans, but it had no effect on the binding of the virus to human receptors. “But the virus has changed subtly,” says Paulson. “Now that mutation causes the change.”
Wilson and Paulson note in their study that the mutated H5N1 protein binds weakly to human receptors but binds more strongly than the 2009 H1N1 virus, which caused the “swine flu” human pandemic. “The initial infection is what we’re concerned about starting a pandemic, and we think the weak association we see with a single mutation is equivalent to a known human pandemic virus,” says Paulson. The study identified a second mutation in a different area of the hemagglutinin, at amino acid position 224, which in combination with the 226 mutation may further enhance the binding ability of the virus.
Guthmiller wasn’t surprised by the findings, given the importance of the 226 mutation in flu receptor preference, but added, “It’s never great when you see just one mutation taking over.” The study “also gives us an idea of what to look for and what areas of the hemagglutinin protein we should focus on to better understand the potential for modification and contamination.”
A teenager in Canada he was recently hospitalized in critical condition due to bird flu with an unknown exposure. Genetic sequencing revealed an H5N1 strain similar to that circulating in Canadian birds, detecting mutations at two positions, one of them was in 226—The same attitude analyzed in the new show. Scientists do not know whether a mutation was responsible for the teenager’s dire condition, but some expressed concern that the changes could be a sign of the virus adapting to human cells.
Paulson says it’s too early to draw conclusions or parallels between the teenager’s case and the findings of the investigation. The amino acids the researchers adjusted in the study were not identical to the viral sequence of the Canadian case, for example, he says. “There’s a lot of jokes about, ‘Oh my gosh, that amino acid is mutating,’ but there’s no evidence yet that this will give us the specificity we would need for human transmission,” Paulson says. But he added that the case is still significant.
Most cases of bird flu in humans reported this year have been mild. In past outbreaks, H5N1 has caused severe respiratory disease because of its preference for binding to cells in the lower respiratory tract, Guthmiller explained. “You’re basically causing viral pneumonia,” he says. “But if you increase the binding to human receptors in the upper respiratory tract,” as this study did, “it’s likely to be more like your common cold … like symptoms.” It’s more likely to spread through sneezing, which could lead to further spread through human contact, he says.
Improved receptor binding does not necessarily cause disease per se. Several other factors are important, such as the ability of the virus to replicate and multiply in the body. But attached to the cells is an initial step, says Paulson. “The magic that we hope doesn’t happen is that all of these things come together so that we have that first (human-to-human) transmission and it becomes a pandemic virus,” he says.

