When I was 17 years old They almost killed me When a fight broke out after a high school football game and someone fired a gun. A stray bullet hit the throat, tore the trachea and damaged the carotid artery.
This afterlife experience traumatized my entire family. However, my parents could not focus solely on my survival and recovery. At the hospital, they were overwhelmed by a maze of paperwork, billing inquiries, and questions about insurance coverage. Even after discharge, challenges continued. Instead of focusing on my recovery, we spent our energy dealing with delayed approvals for follow-up care, denied access to physical therapy, and endless requests for reimbursement clarification.
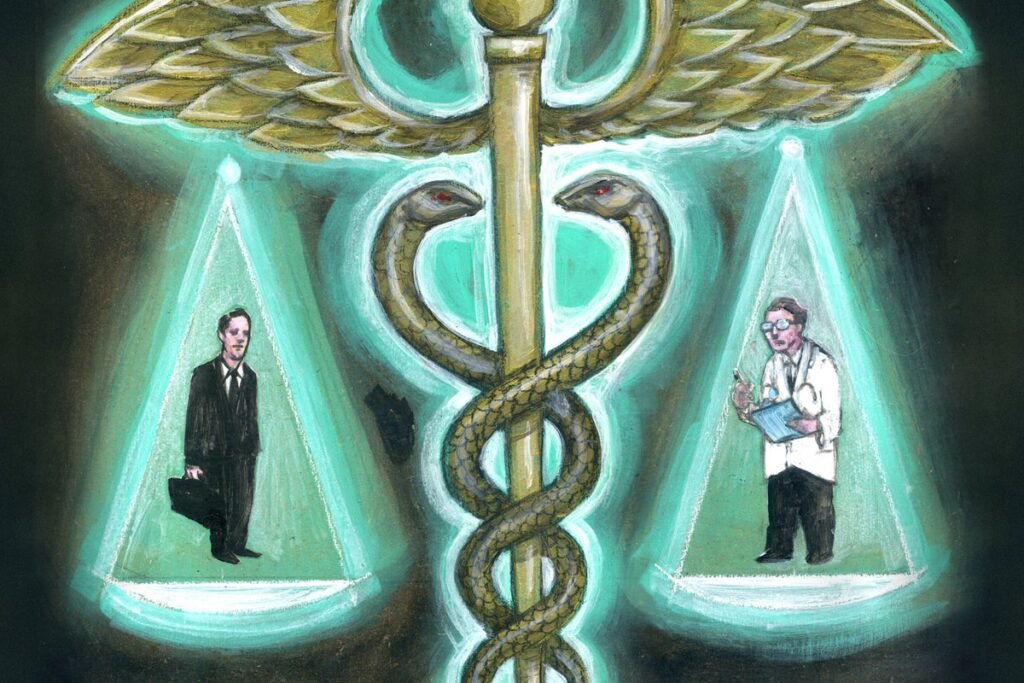
Our health insurance system made a catastrophic time worse for me and my parents. Now, as a trauma surgeon, I have seen how widespread such struggles are. And together The assassination of UnitedHealthcare CEO Brian Thompsonlong and widespread anger over the harm health insurance has caused appears to be boiling over. After decades of public outcry against health policies that put profits over people—policies that deny life-saving treatments, lead to uncovered medical treatment failures, and leave entire communities behind—the call for reform is too loud to ignore. For too many, health insurance is a brick wall: a bureaucratic gatekeeper that creates obstacles rather than solutions.
About supporting science journalism
If you like this article, please consider supporting our award-winning journalism subscribe. By purchasing a subscription, you’re helping to ensure a future of impactful stories about the discoveries and ideas that shape our world.
We cannot justify his murder; so how do we channel our collective grief and frustration into meaningful change? How do we build a healthcare system that provides healing, not harm, a system that values human life over corporate profits? It will take courage, responsibility and will to reimagine a system where patients are seen as people, not financial transactions.
The average annual cost of health care in the US is staggering $15,074 per person. We buy health insurance, on the open market or through our employer, if we need to go to the doctor or undergo treatment, assuming that our insurance will cover most of the expenses—all of them. Yet nearly two-thirds of US bankruptcy is linked to staggeringly high medical expenses, even among people with insurance. around 41 percent Americans are saddled with medical debt, highlighting the system’s profound failure to provide financial security when it is most needed.
In addition to these catastrophic costs—which patients know little about in advance and have little time to understand during medical emergencies—insurance companies also decide whether to pay for care, regardless of whether the patient’s doctor says the care is necessary. Delays in care through bureaucratic hurdles are carefully designed to force people and their doctors to struggle through outdated systems like fax machines and endless phone trees to appeal or request reconsideration of denied treatments or tests. Too often, the mental effort and time spent navigating claims, denials, and appeals wears people down, leading them to forgo getting the coverage they’re owed. This is not inefficiency; it is a predatory failure of empathy for people at their most vulnerable moments. And it increases the anxiety and depression of the patient and their caregivers, increasing the challenges that the system has to deal with.
I have spent countless nights in operating rooms fighting to save lives. I’ve seen how gun violence intersects with health care inadequacies, with families not only grieving but dealing with insurmountable medical bills. Survivors often endure years of physical and financial pain as they deal not only with their injuries, but also with insurance denials for needed care. I know first hand what my patients go through. Every step of my recovery felt like a negotiation, not just for my health, but for access to the care I needed. Sometimes I questioned whether I was seen as a patient or a cost to be managed. These frustrations trickled down to my family, who bore the emotional and logistical burden of dealing with appeals and permits while supporting my recovery.
For many, financial circumstances force impossible choices: families refuse optimal treatment or rehabilitation plans, not because they lack understanding, but simply because they can’t afford them. These compromises lead to worse patient outcomes (and even higher systemic costs), increasing suffering that could have been prevented with adequate access to care. Too often, hope is eroded by a system focused on profit rather than welfare.
To fix this system, we need to fundamentally rethink the principles of care, equity, accountability and cost that underpin it. Cost targeting is essential; it threatens the stability of our health care system, and the financial burden should not fall disproportionately on the people who need health care and their families.
Our policy decisions must reflect our values, so we must ask ourselves: Are we ready to expand coverage so that all Americans have affordable, quality care? Can we accept higher premiums or cost sharing to build a system that ensures subsidies to those who need them most and yet avoids unnecessary or wasted drugs? Beyond coverage, we need to simplify and streamline processes, eliminating unnecessary bureaucratic hurdles that overwhelm patients and families. Equity must be a fundamental pillar, not only in access, but also in the quality of care provided and the financial protections offered.
Mental health should be integrated with physical health and prioritized in care and coverage, recognizing the mind’s key role in the body’s recovery and overall well-being. Excessive profits, rising drug costs, and opaque billing practices in the insurance industry call for accountability and shared responsibility among providers, insurers, pharmaceutical companies, and policymakers. And finally, insurers and clinicians must be held accountable, not for short-term cost reduction, but for improving outcomes, providing compassionate care, and making sure that the patient’s healthcare journey does not lead to financial disaster within reason. If we are serious about building a system that values human dignity over profit, these reforms are not only necessary; they are from a long time ago.
With Donald Trump returning to the presidency, and Republican majorities in both the House and Senate, the likelihood of comprehensive health care reform over the next four years is limited, especially in expanding access through government programs. Instead, the focus is likely to shift further toward deregulation, market-driven solutions, and reducing government involvement in health care, rather than achieving universal coverage or expanding subsidies. Efforts to repeal or further weaken provisions of the Affordable Care Act (ACA) are likely to resurface, along with predatory policies that promote short-term health plans and ineffective state control over Medicaid.
While reducing prescription drug costs may remain a bipartisan goal, broader reforms aimed at equity, simplicity, and expansion of mental health care may stall if they are not aligned with cost-reduction strategies. The challenge will be to ensure that the needs of patients – especially the most vulnerable – are not sidelined between policies that prioritize fiscal conservatism and market efficiency over systemic change.
We urgently need to create a fairer system. Insurers must limit out-of-pocket costs, eliminate lifetime limits and expand income-based assistance so that affected Americans can focus on healing and recovery.
My frustrations with the system shaped my decision to push for positive change. This moment calls for difficult reform and introspection, but it also offers an opportunity for transformation. Our healthcare system should inspire hope, not compound suffering. Patients, clinicians, policy makers, and insurers must all come together to focus on complexity, focus on outcomes, and prioritize people over profits.
This is an opinion and analysis article, and the views expressed by the author(s) are not necessarily their own. American scientific